Introduction
The debate about the clinical role of bathing frequency in atopic dermatitis (AD) has been ongoing for more than 100 years.1,2 Recently, we published data that highlight this debate; primary care physicians more often recommend infrequent bathing, whereas allergists and pediatric dermatologists recommend frequent bathing.3 The lack of consensus has resulted in parental confusion regarding the matter. For instance, we found that among parents who have seen multiple providers for their child’s AD,more than 75% reported a significant amount of confusion and frustration owing to conflicting advice on bathing frequency.4 Considering bathing recommendations often is part of the treatment plan; this parental frustration could negatively affect adherence and thus AD control.
The focus of this article is to summarize and interpret the literature on the role of bathing frequency in patients with AD. For clarity, we define “frequent bathing” as bathing at least once a day and “infrequent bathing” as bathing less than once a day.
Rationale Behind Infrequent vs Frequent Bathing
Confusion about bathing frequency stems from the paradox that water can be good and bad for skin. As Hanifin and Tofte stated,5 bathing followed by evaporation causes stratum corneum contracture and fissures, thereby drying out the skin and impairing the epidermal barrier. They also proposed that bathing, if followed by the application of a moisturizer within 3 minutes, could hydrate the skin and keep the epidermal barrier soft and flexible (this would be termed the “soak and smear” technique).6 There remains disagreement among clinicians regarding the frequency with which patients should bathe, to the frustration of patients and their families.3,4
Several explanations help explain the rationale behind infrequent bathing. Because AD is characterized by xerosis, many clinicians believe that water avoidance is the appropriate way to not further irritate the skin and increase evaporative water losses. Furthermore, frequent bathing is often combined with overuse of detergents (ie, soaps), which can contribute to skin barrier breakdown by increasing stratum corneum pH.7,8 Likewise, routine bathing without application of an emollient can exacerbate xerosis.9 Other factors that could flare AD include high water temperature and physical irritation from excess towel drying or scrubbing of the skin. For these reasons, infrequent bathing has been the preferred approach for many clinicians. This is similar to the patient with hand dermatitis who excessively and aggressively washes the hands with harsh soaps and without appropriate use of emollients. Families often conclude that bathing makes AD worse when their children complain of stinging during the initial exposure to water.
Clinicians who support a frequent bathing approach believe that the presence of xerosis mandates rehydration of the skin with daily baths, limited use of pH-balanced skin cleansers, and gentle patting dry with the immediate application of an emollient after the bath (to “seal” in the added moisture). Indeed, advances in our understanding of skin barrier defects that lead to transepidermal water loss, such as increased skin protease activity in the stratum corneum,7 ceramide deficiency,10 and more recently filaggrin deficiency,11 have formed the justification in favor of frequent bathing.
What Do Guidelines Say?
Limited data regarding the role of bathing frequency in the management of AD has led to guidelines being inconsistent or silent on the topic. A 2003 consensus conference on pediatric AD advocated for once-daily bathing in warm water, using a moisturizing cleanser, and then immediate application of an emollient. The panel reported “there [was] no evidence [at the time] that bathing adversely affects AD if it is performed as outlined.” However, they did call for more studies to better understand the role of bathing and the optimal duration of bathing.12 In the 2009 and updated 2012 European guidelines, experts concluded that, “although bathing seems very important, there is lack of evidence to prove that it is absolutely necessary.” In consequence, they did not comment on bathing frequency but did recommend short 5-minute baths, followed by bath oils in the last 2 minutes, and then emollients applied immediately after patting dry.13,14 Of note, there are no published data evaluating the optimal duration of bathing, and there are scant data for the use of bath emollients, including bath oils within the bath.15,16
Similar to the European guidelines, the United Kingdom’s guidelines in 2007 and the Asia-Pacific guidelines in 2013 did not mention bathing frequency.17,18 In 2009, the Japanese guidelines also did not comment on bathing frequency for routine skin care; but in times of exacerbation, they recommended bathing twice daily with application of topical corticosteroids after the bath.19 The American Academy of Asthma Allergy and Immunology and the American College of Asthma Allergy and Immunology recommended “warm soaking baths for at least 10 minutes (up to 20 minutes) followed by the application of a moisturizer” but did not comment specifically on frequency.20 The American Academy of Dermatology acknowledged that “there is no standard for the frequency or duration of bathing” for those with AD and recommended up to once-daily bathing for 5 to 10 minutes; for significantly inflamed skin, soaking up to 20 minutes followed by the soak and smear technique was recommended.21 Despite the lack of consensus on bathing frequency (and duration), most guidelines recommend rapid application of emollient after bathing and suggest gentle bathing to help eliminate crusts and mechanically decontaminate the skin of bacteria.
Although bathing-related topics, such as the role of emollients, additives, and wet wrap therapy, are not the focus of this review, it is worth mentioning a few words on bleach baths, because it is closely related to the bathing issue, has received much attention in recent years, and has been endorsed by multiple AD guidelines, although not to the same degree.22 Diluted bleach baths have been shown to be a helpful treatment adjunct in cases of moderate to severe disease with frequent bacterial infections.23,24 However, a more recent study did not show clinical improvement compared with placebo.25 As it relates to bathing frequency, subjects underwent bleach baths or placebo bleach baths 2 to 3 times per week. However, the frequency of baths without bleach (or placebo) was not restricted or reported. Therefore, we do not know whether some subjects bathed daily and whether this affected the results. Nevertheless, we do know that clinical improvement occurred only in skin submerged in the bath (not the head and face).23,24
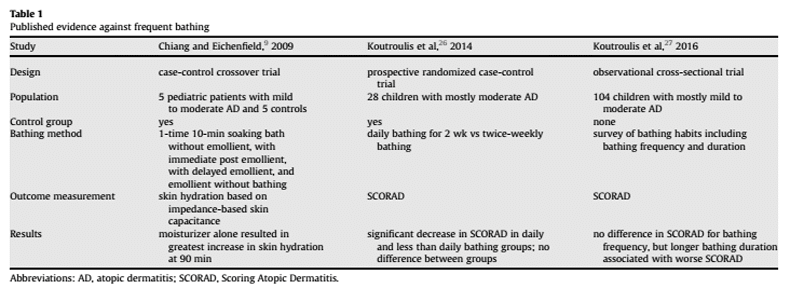
Published Evidence Against Frequent Bathing
Some limited data exist in favor of infrequent bathing (Table 1).9,26,27 Chiang and Eichenfield9 reported that bathing followed by moisturizer application in mild to moderate AD provides only modest hydration benefits, and that simply applying moisturizer without bathing might be more effective based on mean hydration status over 90 minutes. The strength of this study lies in its objective measurement of skin hydration by impedancebased skin capacitance. However, this study was limited by a small sample, and it did not examine clinical symptom scores. Importantly, the study examined the effects after 1 bath and did not consider the potential cumulative effect of bathing over time.
In a prospective 2-week trial comparing daily with less than daily bathing in mostly moderate AD, 28 patients 6 months to 10 years old were randomly assigned to daily bathing (group A) or twice-weekly bathing (group B).26 The investigators found that AD severity, based on the SCORing Atopic Dermatitis score (SCORAD), decreased significantly for the 2 groups compared with baseline, but no difference was found between the groups before and after intervention. The study was limited by a small sample, multiple unblinded physicians measuring SCORAD, lack of methods to ensure adherence, and lack of control for medications and bathing products used before the intervention. It is uncertain whether patients were specifically instructed on the application of emollient within 3 minutes of exiting the bath. In a follow-up study by the same researchers, 104 patients with AD were surveyed to determine whether there was a relation between AD severity and bathing frequency and duration. They found that bathing frequency did not affect SCORAD. However, they found that longer bathing duration was associated with greater AD severity. They acknowledged a potential reporting bias; parents or patients might have reported on bathing and duration based on what they thought they were supposed to say. Likewise, it is unclear as to what the exact bathing practices of the subjects were or what their health care provider might have recommended (eg, their use of emollients after bathing or use of soaps or bubble baths). Whether the patients’ bathing frequency was a cause or result of the severity of AD is unknown.27
Recently, a meta-analysis examined interventional bathing studies and survey studies that assessed patient opinion regarding the use of baths.28 The investigators concluded that repetitive bathing had no beneficial or detrimental effect on AD, and that only a minority of patients with AD favored frequent bathing. The studies used in the analysis excluded trials that did not involve tub baths, baths combined with adjuvant measures, and retrospective studies. Nonetheless, 2 of the 4 studies included still involved the use of bath additives, namely diluted Dead Sea salt solution and
diluted bleach baths. 24,29 The third study looked at infants without existing AD.30 The fourth was by Chiang and Eichenfield.9 Of note, none of the studies reviewed in this analysis (Tables 1 and 2) 6,9,26,27,31e35 that evaluated frequent and/or infrequent bathing were included in their analysis. The investigators suggested plausible explanations for why bathing was not preferred, including the convenience and efficiency of showers over baths and the perception that bathing exacerbates AD. We agree that these are likely reasons why infrequent bathing is preferred, especially when water temperature, bath duration, soaps, and emollients are not controlled for.
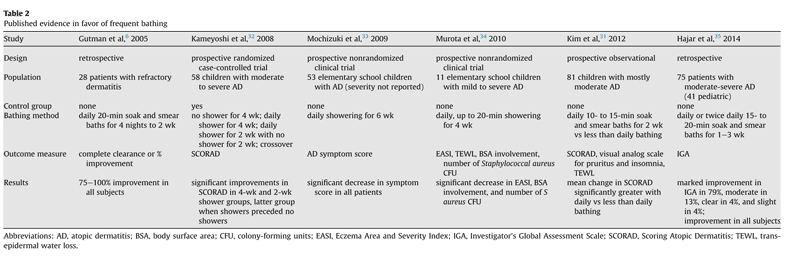
Published Evidence in Favor of Frequent Bathing
The first study advocating for daily bathing was a retrospective study in adults by Gutman et al6 who coined the phrase “soak and smear.” Their data suggested that daily hydration for 20 minutes before bedtime (soak), followed by ointment application (smear), is an effective method to manage certain xerotic skin conditions, including moderate to severe AD. In that study, the use of soak and smear with an anti-inflammatory (for flares) or emollient (for maintenance) was compared with the use of emollient alone. The study did not evaluate pediatric AD and was limited by a small sample and a retrospective design without controls.
In a prospective trial comparing daily with less than daily bathing, 81 patients with AD were asked to perform daily baths for 10 to 15 minutes for 2 weeks followed by emollient application within 3 minutes of patting dry.31 Then, the investigators compared good compliance group A (daily bathing) with poor compliance group B (less than daily bathing) and found that the mean change in SCORAD at 2 weeks was greater in group A than in group B. Group B used statistically insignificant less moisturizer than group A. This was an observational study, with statistical and design limitations.
In another prospective trial of 58 school children with moderate to severe AD, daily showers vs no showers were compared over a 4-week period.32 The investigators found that showers were more effective in significantly improving SCORAD, with the most significant improvements seen in patients with the most severe disease.
These results were replicated in 2 subsequent studies: one involving 53 children over a 6-week period and another involving 11 children over a 4-week period. AD severity scores improved significantly with daily showers; however, these 2 studies were limited by lack of control groups.33,34
In a recent retrospective review of 75 subjects with moderate to severe AD whose high potency topical corticosteroid or systemic therapy had failed, Hajar et al35 found that once- to twice-daily bathing for 15 to 20 minutes, followed by application of a topical corticosteroid, was associated with a high response rate, with most patients exhibiting almost clear or mild level of severity. The study was limited by its retrospective, uncontrolled, unblinded design that did not include an analysis of statistical significance. In addition, the frequency of bathing before presentation was not reported.
What Should We Do in Light of the Uncertainty?
Dr Jon Hanifin has long been considered one of the pioneers and foremost experts on the subject of AD. For years he has advocated for daily bathing and the use of an emollient within 3 minutes of exiting the bath. He has historically recommended a 20-minute soaking bath, but in his opinion, even a brief shower was preferred over infrequent bathing.5
Our opinion is in keeping with that of AD experts such as Dr Hanifin and other clinicians.36 Based on existing, albeit limited, evidence and personal experience, we believe that the aggravation of AD by frequent bathing is more related to the use of detergents and lack of emollient application within 3 minutes of bathing than to the frequency of water exposure. Without immediate emollient application, epidermal dehydration is likely to occur.9 However, if a soak and smear approach is implemented properly, it is an effective management strategy for AD.
Taken together, studies in favor of frequent bathing outnumber those in favor of infrequent bathing, including prospective trials replicated by different groups, explicit bathing instructions requiring soak and smear, and larger cumulative samples. Of the 3 prospective trials that directly compared frequent with infrequent bathing, 2 studies supported daily bathing31,32 and 1 did not.26
Nevertheless, although it is difficult to draw a definitive conclusion from these data, we would recommend a soak and smear frequent bathing approach before a step-up in prescriptive therapy for patients whose AD has not been well controlled and who have been practicing minimal bathing. Conversely, if a patient’s AD is poorly controlled despite bathing frequently, an evaluation for the overuse of detergents and improper or lack of emollient use should be undertaken.
For families who do not desire, believe in, or have the time to bathe daily, we recommend a “shared decision-making” approach.37 For example, if the issue is time, it might be best to demonstrate flexibility so as to not compromise adherence to the overall treatment plan (eg, by recommending soak and smear bathing whenever possible rather than demand daily bathing). If the issue is of not being willing to try or believe in daily bathing, then we would recommend attentive listening and exploring the underlying reasons for these feelings to address them in an empathic and sincere way, thereby fostering relationship-centered care.37
Future Directions
Considering the limitations of these studies, we call on the research community to carry out more randomized controlled trials comparing frequent with infrequent bathing in the treatment of AD. Such studies should be prospective, of large sample size, and single blinded (to eliminate investigator bias regarding bathing). Moreover, preferably 1 individual should assess AD severity (to eliminate interpersonal assessor variability).
In addition, a crossover design would allow for each subject to serve as its own control. Occlusive emollient use also should be controlled for. If a topical anti-inflammatory is used, then it should be the same for all subjects and not be more than low to mid-potency, to avoid a “wash out” of any clinical difference that might be seen from bathing frequency alone. The primary end point should be a validated clinical tool for assessing AD severity (such as SCORAD), because the clinical impact of bathing frequency is the main objective. Secondary end points could include quality of life, skin hydration status, and Staphylococcal aureus colonization burden. Other questions related to bathing frequency also warrant further investigation. These include analyzing the optimal duration and method of bathing (showers vs baths) and whether the effects of bathing relate to allergic sensitization and exposure. Further, our survey of dermatologists consisted mostly of board-certified pediatric dermatologists,3 which make up fewer than 2% of all dermatologists in the United States.38 Therefore, it might be informative to survey general dermatologists not specializing in pediatrics regarding their opinions on bathing frequency, because there are reports that primary care physicians refer their patients with AD more to general dermatologists than to allergists and immunologists.4,39
Conclusion
Despite advances in our understanding of the genetic and immunologic mechanisms behind this common skin condition, there are many basic questions regarding AD management that remain unanswered. Our understanding of the importance of skin barrier function and the role of transepidermal water loss in the pathogenesis of AD underscores the need for clarity on the role of bathing in the management of this condition. Although clinical trials on bathing frequency have shown mixed results, we believe that the weight of the evidence suggests that frequent soak and smear bathing is preferred to infrequent bathing in the management of AD. This simple, low-cost intervention could contribute to better AD control.
Written By:
Ivan D. Cardona, MD, Maine Medical Center, Portland, Maine
Leland Stillman, MD, Maine Medical Center, Portland, Maine
Neal Jain, MD, San Tan Allergy and Asthma
References
[1] Hebra F. Traité des maladies de la peau. Paris: Masson; 1872:567e572.
[2] Besnier E. Traitement de l’eczéma et du psoriasis. Paris: Rueff; 1897:66e83.
[3] Cardona ID, Kempe E, Hatzenbeuhler JR, et al. Bathing frequency recommendations for children with atopic dermatitis: results of three observational pilot surveys. Pediatr Dermatol. 2015;32:e194ee196.
[4] Kempe E, Jain N, Cardona I. Bathing frequency recommendations for pediatric atopic dermatitis: are we adding to parental frustration? Ann Allergy Asthma Immunol. 2013;111:298e299.
[5] Hanifin JM, Tofte SJ. Update on therapy of atopic dermatitis. J Allergy Clin Immunol. 1999;104:S123eS125.
[6] Gutman A, Kligman A, Sciacca J, et al. Soak and smear: a standard technique revisited. Arch Dermatol. 2005;141:155tab6e1559.
[7] Burkhart CG. Clinical assessment by atopic dermatitis patients of response to reduced soap bathing: pilot study. Int J Dermatol. 2008;47:1216e1217.
[8] Cork MJ, Robinson DA, Vasilopoulos Y, et al. New perspectives on epidermal barrier dysfunction in atopic dermatitis: gene-environment interactions. J Allergy Clin Immunol. 2006;118:3e21.
[9] Chiang C, Eichenfield LF. Quantitative assessment of combination bathing and moisturizing regimens on skin hydration in atopic dermatitis. Pediatr Dermatol. 2009;26:273e278.
[10] Sator P-G, Schmidt JB, Hönigsmann H. Comparison of epidermal hydration and skin surface lipids in healthy individuals and in patients with atopic dermatitis. J Am Acad Dermatol. 2003;48:352e358.
[11] O’Regan GM, Irvine AD. The role of filaggrin loss-of-function mutations in atopic dermatitis. Curr Opin Allergy Clin Immunol. 2008;8:406e410.
[12] Eichenfield LF, Hanifin JM, Luger TA, et al. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol. 2003;49:1088e1095.
[13] Darsow U, Wollenberg A, Simon D, et al. ETFAD/EADV eczema task force 2009 position paper on diagnosis and treatment of atopic dermatitis. J Eur Acad Dermatol Venereol. 2010;24:317e328.
[14] Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) part I. J Eur Acad Dermatol Venereol. 2012;26:1045e1060.
[15] Tarr A, Iheanacho I. Should we use bath emollients for atopic eczema? BMJ. 2009;339:b4273.
[16] Bath emollients for atopic eczema. why use them? Drug Ther Bull. 2007;45: 73e75.
[17] Lewis-Jones S, Mugglestone MA. Management of atopic eczema in children aged up to 12 years: summary of NICE guidance. BMJ. 2007;335:1263e1264.
[18] Rubel D, Thirumoorthy T, Soebaryo RW, et al. Consensus guidelines for the management of atopic dermatitis: an Asia-Pacific perspective. J Dermatol. 2013;40:160e171.
[19] Saeki H, Furue M, Furukawa F, et al. Guidelines for management of atopic dermatitis. J Dermatol. 2009;36:563e577.
[20] Schneider L, Tilles S, Lio P, et al. Atopic dermatitis: a practice parameter update 2012. J Allergy Clin Immunol. 2013;131:295e299.e1-27.
[21] Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71:116e132.
[22] Mohan GC, Lio PA. Comparison of dermatology and allergy guidelines for atopic dermatitis management. JAMA Dermatol. 2015;151:1009e1013.
[23] Wong SM, Ng TG, Baba R. Efficacy and safety of sodium hypochlorite (bleach) baths in patients with moderate to severe atopic dermatitis in Malaysia. J Dermatol. 2013;40:874e880.
[24] Huang JT, Abrams M, Tlougan B, et al. Treatment of Staphylococcus aureus colonization in atopic dermatitis decreases disease severity. Pediatrics. 2009; 123:e808ee814.
[25] Hon KL, Tsang YC, Lee VW, et al. Efficacy of sodium hypochlorite (bleach) baths to reduce staphylococcus aureus colonization in childhood onset moderate-to-severe eczema: a randomized, placebo-controlled cross-over trial. J Dermatolog Treat. 2016;27:156e162.
[26] Koutroulis I, Petrova K, Kratimenos P, et al. Frequency of bathing in the management of atopic dermatitis: to bathe or not to bathe? Clin Pediatr (Phila). 2014;53:677e681.
[27] Koutroulis I, Pyle T, Kopylov D, et al. The association between bathing habits and severity of atopic dermatitis in children. Clin Pediatr (Phila). 2016;55:176e181.
[28] Sarre ME, Martin L, Moote W, et al. Are baths desirable in atopic dermatitis? J Eur Acad Dermatol Venereol. 2015;29:1265e1274.
[29] Proksch E, Nissen H-P, Bremgartner M, et al. Bathing in a magnesium-rich Dead Sea salt solution improves skin barrier function, enhances skin hydration, and reduces inflammation in atopic dry skin. Int J Dermatol. 2005;44:151e157.
[30] Lavender T, Bedwell C, O’Brien E, et al. Infant skin-cleansing product versuswater: a pilot randomized, assessor-blinded controlled trial. BMC Pediatr. 2011;11:35.
[31] Kim H, Ban J, Park M-R, et al. Effect of bathing on atopic dermatitis during the summer season. Asia Pac Allergy. 2012;2:269e274.
[32] Kameyoshi Y, Tanaka T, Mochizuki M, et al. [Taking showers at school is beneficial for children with severer atopic dermatitis]. Allergy. 2008;57:130e137 [in Japanese].
[33] Mochizuki H, Muramatsu R, Tadaki H, et al. Effects of skin care with shower therapy on children with atopic dermatitis in elementary schools. Pediatr Dermatol. 2009;26:223e226.
[34] Murota H, Takahashi A, Nishioka M, et al. Showering reduces atopic dermatitis in elementary school students. Eur J Dermatol. 2010;20:410e411.
[35] Hajar T, Hanifin JM, Tofte SJ, et al. Prehydration is effective for rapid control of recalcitrant atopic dermatitis. Dermatitis. 2014;25:56e59.
[36] Ong PY. To bathe or not to bathe in atopic dermatitis. American Academy of Pediatrics California Chapter 2 Newsletter. 2005.
[37] Ring L, Kettis-Lindblad A, Kjellgren KI, et al. Living with skin diseases and topical treatment: patient’s and providers’ perspectives and priorities.J Dermatolog Treat. 2007;18:209e218.
[38] Prindaville B, Antaya RJ, Siegfried EC. Pediatric dermatology: past, present, and future. Pediatr Dermatol. 2014;32:1e12.
[39] Convers KD, Slavin RG. Attitudes toward allergy: what do the pediatricians think? Ann Allergy Asthma Immunol. 2014;113:544e548.